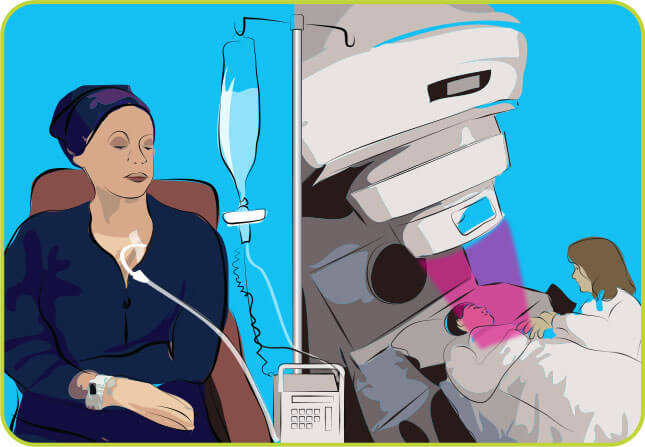
The idea behind autologous hematopoietic cell transplantation (autologous HCT) is to allow administration of higher chemotherapy and/or radiation therapy doses to kill cancerous cells, then replenish bone marrow cells, white blood cells (WBCs), red blood cells (RBCs), and platelets.
Patient & Caregiver Education Booklet. 4.25MB
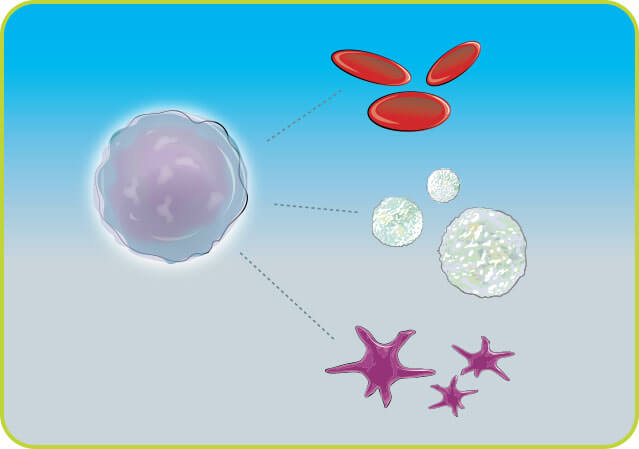
Hematopoietic stem cells (referred to in this website as stem cells) are unique cells that are primarily located in the bone marrow and mature into a number of blood cell types found in your body. This includes red blood cells, which carry oxygen to, and carbon dioxide away from, the body's tissues; white blood cells, which fight bacteria, viruses and fungi that can cause infection; and platelets, which aid in the blood clotting process.
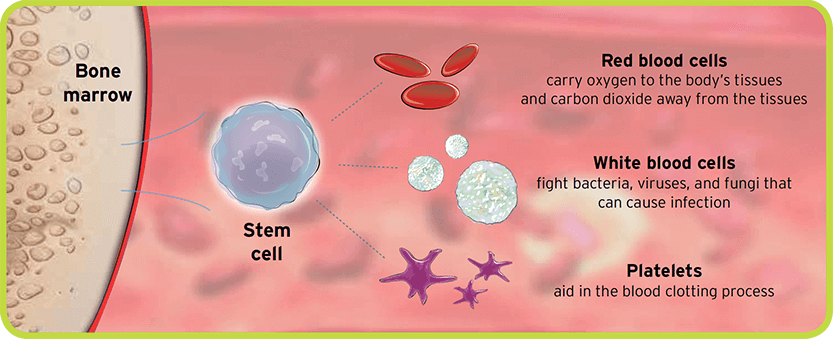
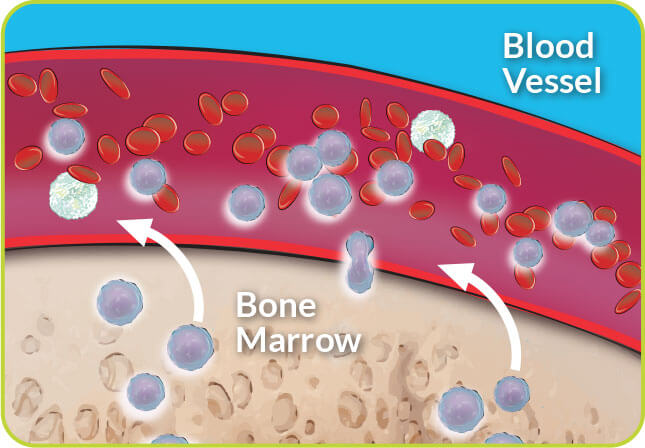
In adults, the bones of the hip and chest contain the greatest amount of bone marrow and stem cells. Stem cells that leave the bone marrow and circulate into the bloodstream are called peripheral blood stem cells (PBSCs). Although very few PBSCs are found in the bloodstream (outside the bone marrow space), their numbers can be increased through administering mobilization agents.
HCT can be a complicated process. If your doctor has recommended an autologous HCT for you or your family member, it’s important to know what to expect as you prepare for this process.
Although there are very few peripheral blood stem cells, their numbers can be increased through administering medications such as filgrastim, chemotherapy, and agents like Mozobil (plerixafor) injection.
Mozobil is a drug that in combination with filgrastim increases stem cells in the blood that can be collected for autologous HCT in patients with NHL or MM. Mozobil is not intended for HCT mobilization and collection in patients with leukemia.
Learn about the benefits and risks of Mozobil in HCT mobilization.
Your doctor and transplant team will determine a mobilization regimen for you to help release your stem cells out of the bone marrow into the bloodstream for collection.
See details of the stem cell mobilization process.
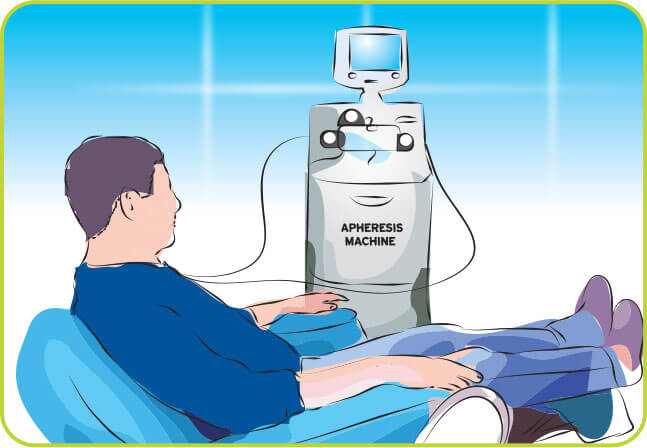
During peripheral blood stem cell collection, you will be connected to an apheresis machine, also known as a cell separator. Blood will leave your body through a central venous catheter (CVC), the machine will collect the stem cells and then the remaining blood components will return to your body through the catheter. A blood thinner called citrate may be slowly added to your blood during this process to help prevent blood clotting.
This process may take approximately 4–6 hours to complete each day. Repeated collections on subsequent days may be needed to collect enough stem cells for your transplant.
Your stem cells will be processed, frozen, and stored after each apheresis session. Your frozen stem cells will be ready and waiting for you once you have completed your chemotherapy and/or radiation.
During the freezing process, a chemical call dimethylsulfoxide (DMSO) is mixed with the stem cells to protect the cells during freezing.

After the stem cells are collected, you will receive high-dose chemotherapy and/or radiation therapy. These higher doses of chemotherapy and radiation are intended to kill any remaining cancer cells and make room for your new cells to grow. The side effects that may occur during this phase may be similar to those you experienced with previous treatment, but could range in severity.
On the day of your autologous HCT, the frozen, previously collected stem cells will be brought to your bedside, thawed, and infused back into your bloodstream through your CVC. Infusion times range from 30 minutes to 5 hours, depending upon the volume of cells to be infused. During and for a period after the infusion, you will be checked frequently for signs of fever, chills, hives, a fall in blood pressure, and/or shortness of breath, among other potential side effects.

As soon as your stored stem cells are infused, they travel through your bloodstream to the bone marrow space in a process called homing.
Even though the stem cells start the homing process right away, it will be approximately 8–30 days before these infused cells are able to mature and produce healthy new blood cells, a process called engraftment.
Ask your doctor about the details of your transplant process. Use the discussion guide below to start the conversation.